
MIG Update – July 24, 2023
Varriano Appeal Quoted in MIG Case
This week’s case, a MIG hold where the applicant failed to establish they suffered non-minor injuries. However, the Tribunal was instructive on the application of Varriano where medical and any other reasons were required in response to the disputed treatment plan for a chronic pain assessment.
LAT Update – What Difference Did A Year Make?
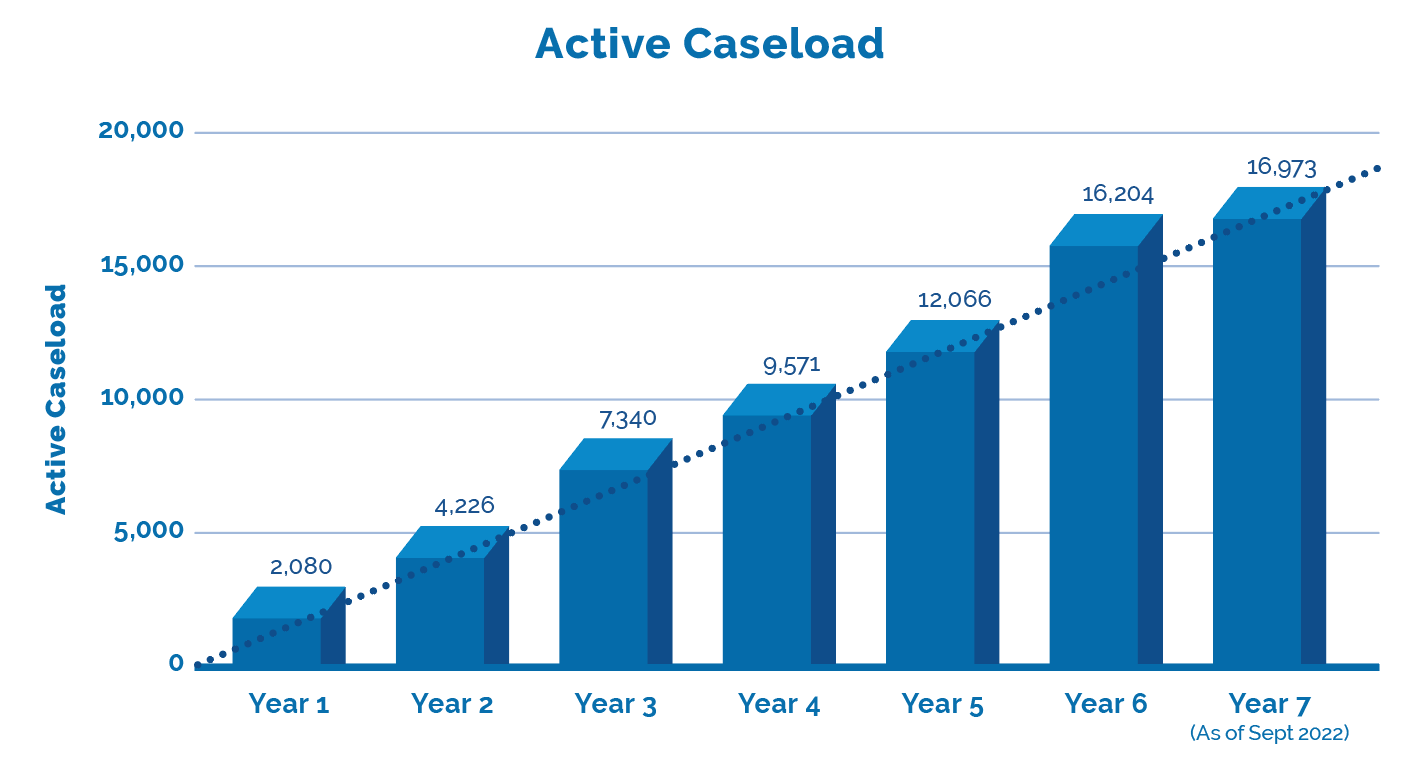
The LAT released Performance Stats up to mid-year 7 which is current through to the end of September 2022. Together with the LAT’s last update we can now provide a comparison of year over year, with projections through to the end of year 7 in this annual update. What difference did a year make?
Factor: “Varriano” Test For Medical Reasons
In Felix v. The Personal Insurance Company (21-001201), Christine Felix was involved in an automobile accident on February 15, 2019, and sought benefits including a chronic pain assessment. Felix submitted that she was diagnosed with chronic pain and had a documented pre-existing medical condition that would remove her from the MIG.
The Personal relied on the evidence of their assessors Dr. El-Hage and Dr. D’Souza in support of their position that Felix had not established that she met the criteria for chronic pain syndrome and a pre-existing condition. Dr. D’Souza concluded that Felix sustained soft tissue injuries and only met the criteria under item 3 (physical deconditioning) and opined Felix’s injuries fell within the MIG. The Tribunal agreed.
Felix’s family doctor, Dr. Lei’s records had 3 entries with the first being 13 months after the accident noting some low back pain,, no diagnosis or referrals were made and the records were silent on any psychological issues.
Turning to the chronic pain assessment proposed by Excel Medical Diagnostics, in a treatment plan dated February 26, 2020 and denied on March 26, 2020. The Personal’s denial notice set out these reasons:
“I received recommendations dated Feb. 26, 2020 from Excel Medical Diagnostics Inc. The total recommendation of $2,460.00 has not been approved because I believe your injuries are categorized as Minor Injury. Recommendations must address your diagnosis. I provided some guidance below in ‘Additional details’ to help you understand the minor injury category.
I reviewed your list of injuries and see no pre-existing conditions described. In comparing your injuries to the criteria in the Minor Injury Guideline, I’ve concluded your injuries are minor and fall within the Guideline. 18(1) of the Statutory Accident Benefits Schedule sets a policy limit for minor injuries. I am unable to approve the recommendations because I’ve paid the maximum amount”.

It is noteworthy to quote the Tribunal specifically at para 35:
Both parties rely on the decision of the Divisional Court in Varriano v. Allstate, 2021 ONSC 8242 (“Varriano”), which discussed the sufficiency of notice and meaning of “medical and other reasons”. In summarizing previous Tribunal cases, the Divisional Court noted that the insurer should comply with the following “imminently reasonable baseline standards” when providing valid notice:
a) explain its decision with reference to the insured’s medical condition and any other applicable rationale;
b) include specific details about the insured’s condition forming the basis for the insurer’s decision or, alternatively, identify information about the insured’s condition that the insurer does not have but requires;
c) refer to the specific benefit or determination at issue, along with any section of the SABS upon which it relies; and
d) be clear and sufficient to allow an unsophisticated person to make an informed decision to either accept or dispute the decision at issue.
The Court of Appeal recently overturned the order of the Divisional Court in Varriano, however the question on appeal was whether insurers always have to provide a “medical reason” if they have also already provided “any other reason”. The Court of Appeal did not comment on the above standards. I find that there is no reason to disregard the Divisional Court’s summary above, and that it is a helpful tool for analysis.
- The Personal failed to provide proper notice in accordance with s. 38(8) of the Schedule and the Treatment Plan triggering the consequences of s. 38(11)2 of the Schedule. Since the assessment was completed the cost of same plus interest was found payable.
- The Personal’s denial failed to list Felix’s injuries, or state what medical or other documents it reviewed or was relying on. Their notice letter failed to satisfy the first, second, and fourth principles listed above.
- It was not enough to simply list the criteria in the MIG without any further reference to how Felix’s injuries fit within it. An unsophisticated person would not have any idea what the The Personal relied on to make its determination.
If you Have Read This Far…
Our MIG Monday series discusses the multitude of factors to consider when evaluating a risk position on MIG cases. The Tribunal has ruled on the MIG in 24% of the decisions so far. Each case is nuanced, but with similar factors.
Inform your position & present persuasive arguments. Include an Outcome Analysis Report (OAR) in your case evaluation complete with For/Against cases. Need an OAR?
inHEALTH Keeps you LAT inFORMED With Access To:
1. LAT Compendium Database – a relational database of LAT and Divisional Court Decisions equipped with multiple search options, Smart Filters, and concise case summaries
2. Notifications: – weekly LAT inFORMER delivered to your inbox Wednesdays; Newly Added Decisions on Fridays and Breaking News as and when it happens
3. Research Support: – inHEALTH’s Live Chat Experts for guided searches and technical inquiries.
Sign up for a 14 day free trial below to experience the service and see how it can help guide your decision making.